Diabetes is a growing health concern worldwide, and understanding the differences between Type 1 diabetes and Type 2 diabetes is vital for effective management and prevention. Each type of diabetes presents unique characteristics, causes, and treatment approaches. Recent studies indicate that the prevalence of Type 2 diabetes, largely driven by lifestyle factors, is on the rise, impacting millions globally.
Type 1 diabetes is an autoimmune condition that typically develops in children and young adults, while Type 2 diabetes is more common in adults and is often linked to obesity and sedentary lifestyles. Recognizing these differences not only helps in promoting awareness but also assists individuals in making informed decisions regarding their health. This post aims to clarify these distinctions, enabling readers to better understand their own experiences with diabetes.
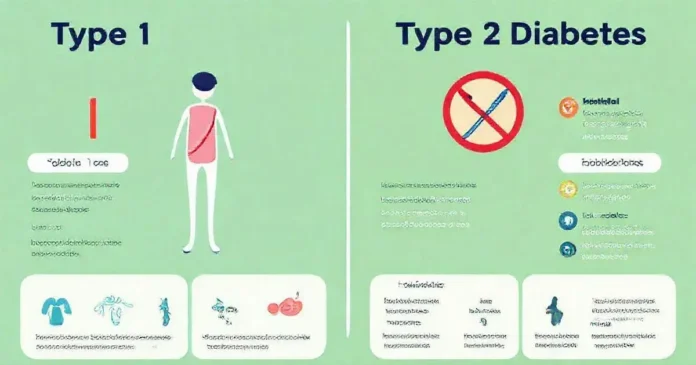
Key Differences Between Type 1 and Type 2 Diabetes
Understanding diabetes is crucial for managing this condition effectively. Type 1 and Type 2 diabetes are distinct types, and recognizing their differences can help patients and caregivers make informed decisions. Type 1 diabetes is primarily an autoimmune disorder where the pancreas produces little to no insulin. It often develops in childhood or adolescence. In contrast, Type 2 diabetes is more associated with insulin resistance and typically develops later in life.
Another critical difference lies in the cause. While Type 1 is usually genetic and sometimes triggered by environmental factors, Type 2 is heavily influenced by lifestyle choices such as diet and physical activity. Therefore, addressing lifestyle changes can effectively manage Type 2 diabetes.
The age of onset also varies. Type 1 diabetes can appear suddenly in children or young adults, while Type 2 diabetes generally emerges in adults, often linked with obesity and inactivity. The approach to treatment differs based on these distinctions.
Insulin dependency is vital when contemplating treatment options. Individuals with Type 1 diabetes will rely on insulin injections or pumps for life. On the other hand, Type 2 patients might manage their condition through oral medications, insulin, or lifestyle changes. This difference emphasizes the personalized approach required for each patient.
To summarize, knowing these key differences can facilitate better conversations with healthcare providers. A reliable app, such as MySugr, can help users keep track of their type, symptoms, and management strategies effectively.
Symptoms and Diagnosis of Type 1 and Type 2 Diabetes
The symptoms of diabetes can be subtle and often go unnoticed in the early stages of the disease. For both Type 1 and Type 2 diabetes, common symptoms include excessive thirst, frequent urination, extreme fatigue, and blurred vision. However, symptoms in Type 1 diabetes might develop more rapidly, sometimes even within a few weeks.
Diagnosis often requires a series of blood tests. The A1C test measures average blood glucose levels over the past two to three months. For Type 1, low insulin levels may be noted, while Type 2 typically shows insulin resistance. The American Diabetes Association (ADA) website is a valuable resource for understanding these tests and their interpretations.
Self-monitoring can help catch symptoms early. Using apps like Glucose Buddy, patients can log their symptoms, diet, and glucose levels. This information assists healthcare providers in making accurate diagnoses and tailoring treatment plans.
It’s essential for individuals at risk to undergo regular screening. For Type 1 diabetes, family history plays a significant role, while Type 2 can be detected through routine physical examinations and blood tests, particularly for those who are overweight or have a sedentary lifestyle.
Ultimately, the identification and diagnosis of diabetes types involve understanding one’s own body and working closely with healthcare professionals. Websites like the CDC provide guidelines on what symptoms to monitor and when to seek medical advice.
Managing Type 1 and Type 2 Diabetes Effectively
Effective management of diabetes is paramount for maintaining quality of life. For Type 1 diabetes, daily insulin management is critical. Patients must calculate their carbohydrate intake and match their insulin doses accordingly. Using apps like Carb Manager can aid in tracking food intake and calculating insulin needs.
Type 2 diabetes management leans heavily on lifestyle adjustments. Regular exercise, a balanced diet, and weight management play significant roles. Tools like MyFitnessPal help users cultivate healthier eating habits while monitoring their physical activities.
Continuous glucose monitors (CGMs) can significantly enhance management strategies for both types. Devices such as Dexcom G6 provide real-time glucose readings, enabling patients to make timely decisions regarding food or insulin. Integrating these technologies is crucial for effective diabetes management.
Education and support networks are essential. Joining support groups or attending diabetes education classes can provide valuable information and foster community connections. Websites like Diabetes.org offer resources for finding local support groups.
Lastly, regular check-ups with healthcare providers are indispensable. Patients should create a scheduled plan for monitoring their diabetes, discussing their management strategies, and making necessary adjustments as needed. By utilizing apps, resources, and education, managing diabetes becomes a structured and successful endeavor.
Causes of Type 1 and Type 2 Diabetes Explained
Understanding the causes of type 1 diabetes and type 2 diabetes is essential for anyone looking to manage or prevent these conditions. Type 1 diabetes is primarily an autoimmune disorder. In this scenario, the body’s immune system mistakenly attacks the insulin-producing beta cells in the pancreas. This process leads to little or no insulin production, which is crucial for regulating blood sugar levels. The exact trigger for this autoimmune response is not fully understood, but genetic predisposition often plays a role.
Conversely, type 2 diabetes has different underlying causes. This form of diabetes is largely associated with lifestyle factors such as obesity, poor diet, and physical inactivity. Insulin resistance occurs when the body’s cells cannot use insulin effectively, leading to higher blood sugar levels. Over time, the pancreas tries hard to compensate for the increased demand for insulin, which can eventually lead to its dysfunction.
Environmental factors and genetics can also influence the development of type 2 diabetes. Individuals with a family history of this diabetes are at a higher risk, but lifestyle modifications can sometimes prevent the onset. To mitigate risks, maintaining a healthy weight through balanced nutrition and regular physical activity is crucial. Eating a diet rich in whole grains, fruits, and vegetables while limiting sugars and refined carbs is beneficial.
For both types of diabetes, age can be a contributing factor. Type 1 diabetes often appears in childhood or adolescence, while type 2 diabetes is more prevalent in adults, particularly those over 45. Additionally, certain ethnic groups are more susceptible to type 2 diabetes, which highlights the interplay between genetics and environment.
Understanding these causes can empower individuals to take preemptive measures and make informed decisions regarding their health. Regular health check-ups and consultations with healthcare providers will facilitate timely interventions and lifestyle changes to manage or prevent type 1 diabetes and type 2 diabetes effectively.
Life Expectancy Insights for Type 1 and Type 2 Diabetes
Life expectancy for individuals with type 1 diabetes and type 2 diabetes is a significant concern and varies greatly between the two types. Type 1 diabetes has traditionally been associated with a shorter life expectancy. This is primarily due to complications that can arise from the condition, including heart disease, kidney failure, and neuropathy. However, advancements in medical care and technology have made it increasingly possible for individuals with type 1 diabetes to live long, healthy lives.
In contrast, type 2 diabetes often develops later in life and can be more manageable through lifestyle changes. Studies indicate that individuals with type 2 diabetes can achieve a life expectancy close to their non-diabetic peers, provided they maintain healthy blood sugar levels and manage their condition effectively. Critical to this is adhering to treatment plans, which may include medications, regular exercise, and dietary adjustments.
The management of diabetes plays a vital role in life expectancy. For those with type 1 diabetes, continuous glucose monitoring and advancements in insulin delivery systems are helping patients control their blood sugar levels more efficiently, reducing the risk of severe complications. For type 2 diabetes, lifestyle interventions like weight management and increased physical activity are key strategies for improving health outcomes.
Moreover, psychological aspects cannot be overlooked. Mental health significantly influences diabetes management. Stress and depression can adversely affect one’s ability to control blood sugar levels. Thus, support systems, therapy, and education on diabetes can contribute positively to life expectancy and overall quality of life.
Ultimately, both type 1 diabetes and type 2 diabetes require individualized management strategies to optimize life expectancy. The combination of medical interventions, lifestyle choices, and emotional support creates a holistic approach focused on improving the duration and quality of life for individuals affected by diabetes.
Common Myths About Type 1 and Type 2 Diabetes Debunked
Misinformation about type 1 diabetes and type 2 diabetes can lead to unnecessary confusion and stigma. One prevalent myth is that people with type 1 diabetes can lead normal lives without any health concerns, as they manage their condition. While managing type 1 diabetes effectively is possible, the reality is that individuals require constant monitoring and insulin administration. This myth downplays the challenges that many face daily.
Another common misconception is that type 2 diabetes only affects older adults. While age is a significant risk factor, type 2 diabetes is increasingly being diagnosed in younger individuals, largely due to rising obesity rates and sedentary lifestyles among children and teens. Educating the public about this changing landscape is essential in combating type 2 diabetes.
Some believe that people with diabetes cannot eat sugar at all. While it’s true that individuals with type 1 diabetes and type 2 diabetes need to maintain stable blood sugar levels, they can consume sugar in moderation. The key is managing overall carbohydrate intake, not completely eliminating sugars from the diet.
A myth that persists is that type 2 diabetes is not serious or can be managed solely through diet and exercise. While lifestyle changes are crucial, many people eventually require medication or insulin therapy to control their blood glucose levels effectively. This misconception can lead to individuals not taking their condition seriously or neglecting necessary medical care.
Lastly, there’s a belief that insulin is a cure for diabetes. While insulin therapy is vital for managing type 1 diabetes and may benefit some with type 2 diabetes, it is not a cure. Diabetes management is an ongoing process that encompasses various treatments, lifestyle changes, and regular monitoring. Addressing these myths and providing accurate information can empower individuals to take charge of their diabetes management and improve their overall health.
conclusão
In summary, understanding the differences between type 1 and type 2 diabetes is crucial for management and prevention. Type 1 diabetes is an autoimmune condition where the body fails to produce insulin due to the destruction of pancreatic beta cells. In contrast, type 2 diabetes, often linked to lifestyle choices like diet and exercise, involves insulin resistance and can, in some cases, be prevented or managed with lifestyle changes. Recognizing the importance of these distinctions can empower individuals to make informed decisions regarding their health and wellness.
Life expectancy varies notably between individuals with type 1 and type 2 diabetes. While type 1 diabetes has been associated with a shorter life expectancy primarily due to complications, advancements in medical care have improved outcomes significantly. On the other hand, people with type 2 diabetes can achieve life expectancy similar to their non-diabetic counterparts through proactive management and healthful lifestyle choices. This highlights the importance of adhering to treatment plans which include medication, regular physical activity, and healthy eating.
Lastly, debunking common myths surrounding diabetes is vital to reduce stigma and misinformation. Understanding that both types of diabetes require ongoing management, rather than viewing them as conditions that can be ignored or easily controlled by diet alone, is crucial. Moreover, recognizing that insulin is not a cure but an essential tool for managing these conditions empowers people to engage actively in their treatment plans. By addressing these myths and myths while promoting education about diabetes, we can better support individuals living with diabetes and enhance their quality of life. This holistic approach, coupled with support systems for mental well-being, will ultimately contribute to improved health outcomes for those affected.